Depression is common following brain injuries such as stroke and traumatic brain injury, nearly double that of people without brain injuries. However, research on effective therapies for depression after brain injury is lacking, with brain injury survivors rating mental health difficulties as their number one long-term unmet need.
Cognitive disabilities, such as memory and planning skills difficulties, are common after brain injury and are prevent benefit from standard “talking therapy” approaches available in the NHS. Andrea Kusec and colleagues at the MRC Cognition and Brain Sciences Unit (MRC CBU), investigated ways to make depression therapies more accessible for those with cognitive disabilities. “Behavioural Activation”, a therapy focused on engaging in rewarding activities like contacting a friend or hobbies, was adapted with cognitive strategies to encourage memory for and attention to these activities to “boost” mood benefits.
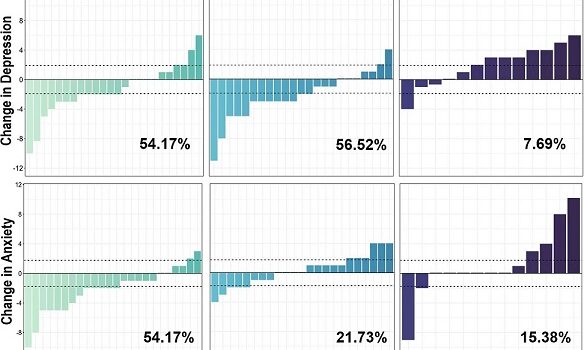
Compared to those not receiving this augmented therapy, about 60% of brain injury survivors had clinically significant improvements in daily activities, mood, anxiety and motivation. This is an important finding because tailoring the therapy to the participants’ needs made for a stronger and more accessible treatment for brain injury survivors with cognitive disability. Given its straightforward approach, this augmented therapy can be easily-trainable across NHS services.
Kusec, A., Murphy, F.C., Peers, P.V. et al. Mood, Activity Participation, and Leisure Engagement Satisfaction (MAPLES): results from a randomised controlled pilot feasibility trial for low mood in acquired brain injury. BMC Med 21, 445 (2023). https://doi.org/10.1186/s12916-023-03128-7

 MRC Cognition and Brain Sciences Unit
MRC Cognition and Brain Sciences Unit